After an IVF cycle fails, many couples become confused and try to determine whether the embryo or the uterus caused the failure.
This debate about embryo quality versus uterus is quite frequent, but the actual situation requires a more intricate assessment.
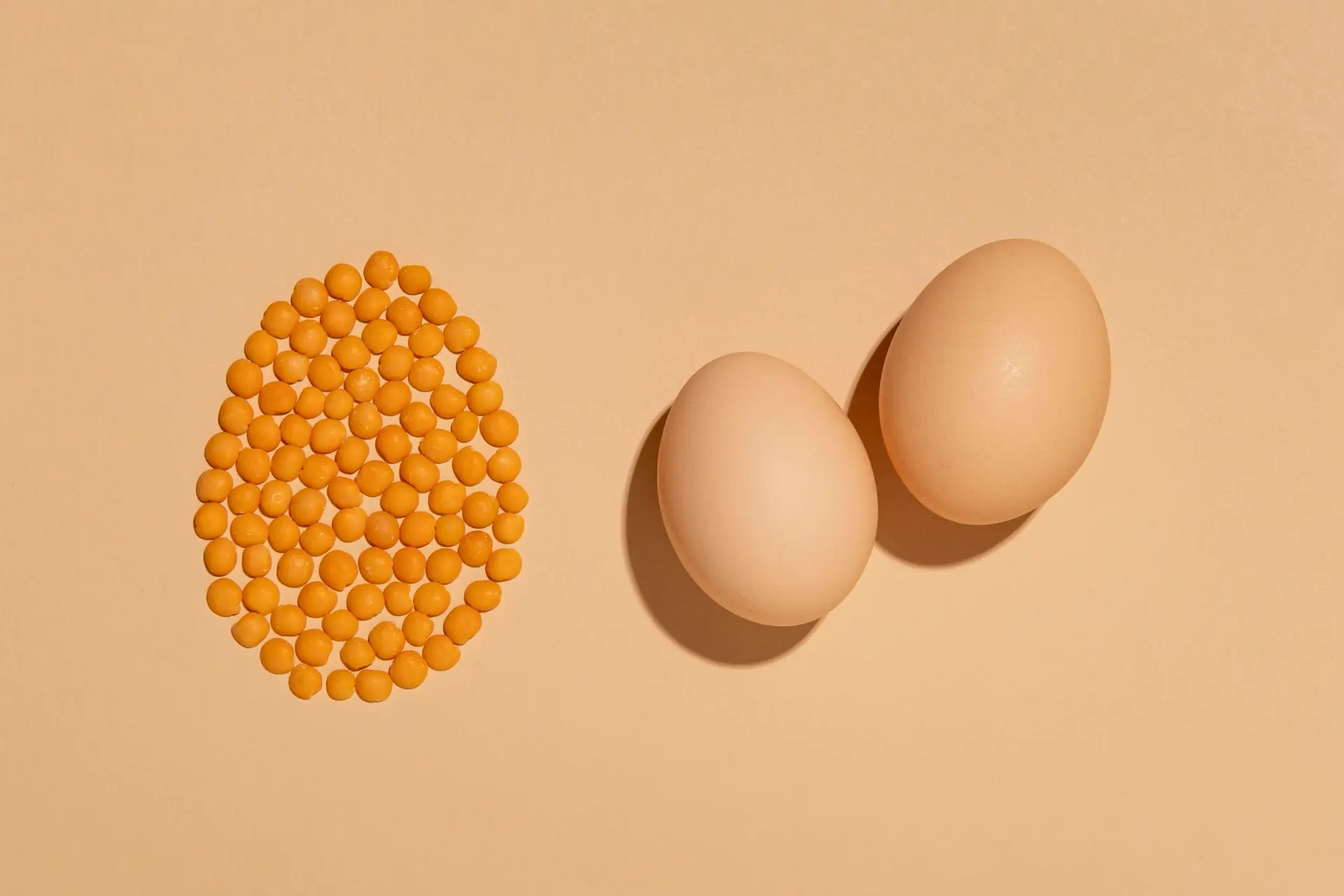
Successful IVF requires two conditions: a healthy embryo and a supportive uterine environment for implantation. Understanding the balance between embryo health and uterine factors IVF is crucial for improving outcomes and avoiding repeated disappointment.
Why IVF Can Fail Even With Good-Quality Embryos
Embryo grading relies on the examination of an embryo under a microscope, but morphology does not always reflect genetic competence. Implantation represents a complex biological process.
The problem exists either due to chromosomal abnormalities or an unreceptive uterine lining. The process fails when either the embryo or the uterus fails to function in synchrony with each other.
Understanding Implantation Failure in IVF
The term “implantation failure causes” refers to reasons why an embryo does not successfully attach to the uterine lining after transfer. The process of implantation requires the presence of:
- A genetically competent embryo
- A receptive, well-prepared endometrium
- Proper hormonal support
- A healthy uterine environment
When Embryo Quality Is the Primary Issue
The primary concern in most situations involves embryo-related elements that mainly affect women who are 35 years old and older. The advancement of age reduces the quality of eggs resulting in negative effects on embryonic development.
The most frequent reason for implantation failure arises from chromosomal abnormalities (aneuploidy). Genetic errors exist in all perfectly graded embryos that create obstacles for successful implantation and increase the risk of early miscarriage.
The central problem with embryo competencies can occur through three specific patterns: repeated poor blastocyst formation, low fertilization rates, and multiple biochemical pregnancies.
Genetic and Developmental Factors in Embryos
Embryos must undergo several critical developmental steps before implantation.
- Cell division must occur properly
- The embryonic genome needs to start working
- A suitable blastocyst must be developed
- The process needs to maintain chromosomal stability
Any of these stages needs to achieve complete success because all of them actually lead to implantation failure. Sperm DNA integrity also plays a role in embryo development, highlighting that IVF outcomes are not solely dependent on the female partner.
Genetic testing (such as PGT-A) may help identify embryos with normal chromosomal patterns, particularly in cases of repeated IVF failure.
When the Uterus Is the Missing Piece
The medical field uses the term “uterine factors IVF” to investigate cases where high-quality embryos fail to implant. A uterus that appears normal on routine ultrasound may still harbor subtle issues affecting receptivity. The endometrium needs to achieve a specific state for implantation to take place that creates a “window of implantation” period. The system requires precise timing because even small changes will disrupt its operations.
Structural Uterine Factors Affecting Implantation
Structural problems are significant implantation failure causes. These include:
- Endometrial polyps
- Submucosal fibroids
- Uterine septum
- Intrauterine adhesions (Asherman’s syndrome)
Even minor intrauterine abnormalities can disrupt implantation by altering blood flow or preventing proper embryo attachment. Many of these issues are undetectable on basic scans and require direct visualization for diagnosis.
Inflammation and Endometrial Health
Chronic endometrial inflammation/chronic endometritis can silently disrupt the implantation process. The inflammatory environment prevents embryo attachment despite the absence of symptoms.
The endometrial microbiome and immune imbalances now serve as recognized factors that contribute to reproductive issues.
Embryo Quality vs Uterus: Why One Cannot Be Ignored
The discussion of “embryo quality vs uterus” should not be framed as an either/or debate. IVF success depends on synchrony between the two. The first step to achieving better embryo quality involves optimizing stimulation protocols and conducting genetic screening.
But, transferring even a genetically normal embryo into an unreceptive uterus will still result in failure. A chromosomally abnormal embryo cannot be rescued by perfect uterine conditions.
The comprehensive evaluation method examines both elements simultaneously instead of attributing responsibility to only one element.
The Role of Hysteroscopy in IVF Evaluation
People frequently underrate the importance of hysteroscopy’s role in IVF procedures. Hysteroscopy allows direct visualization of the uterine cavity and is considered the gold standard for diagnosing structural abnormalities. The system identifies:
- Small polyps
- Subtle adhesions
- Septa
- Chronic inflammatory changes
Hysteroscopy’s role in IVF is crucial and provides immediate results that enable doctors to proceed with necessary treatments for patients specially suffering from persistent IVF failures.
Why Repeating IVF Without Re-evaluation Often Fails
Couples undergo multiple IVF cycles with identical protocols. The same outcome happens because people fail to identify specific reasons that prevent implantation from occurring.
Rather a thorough examination should be performed to determine whether embryo competence or uterine receptivity or their combination requires assessment. Customization and personalized reassessment increases the probability of successful results in upcoming transfer procedures.
How Luma fertility Identifies the Real Cause of IVF Failure
The medical specialists conduct thorough evaluations which go beyond basic assumptions.
The team studies:
- Embryo development patterns
- Genetic testing results
- Endometrial thickness and timing
- Structural assessment through hysteroscopy
- Inflammatory markers where indicated
Implantation Failure Needs Answers, Not Assumptions
Failed IVF cycles are emotionally and physically exhausting. But, assigning blame to either the embryo or uterus without investigation can delay the right solution.
When failure occurs, it demands careful diagnosis, not guesswork.
For a successful pregnancy, an understanding of the embryo competence, uterine factors IVF, or both would be the foundation for moving forward confidently and improving the chances of a successful pregnancy.
FAQs
What are the most common implantation failure causes?
The most common implantation failure causes include poor embryo genetics, uterine abnormalities, inflammation, and hormonal timing issues.
How do uterine factors affect IVF success?
Uterine factors IVF cases involve structural, inflammatory, or receptivity problems that can prevent a healthy embryo from attaching.
Can IVF fail because of the uterus even with good embryos?
Yes, IVF can fail if the uterus is not receptive, even when transferring good-quality embryos.
What is the role of hysteroscopy in IVF?
The hysteroscopy IVF role is to directly examine and treat uterine cavity issues that may interfere with implantation.
Is embryo quality more important than the uterus?
In the embryo quality vs uterus debate, both are equally critical because implantation requires a healthy embryo and a receptive uterine lining.
When should uterine evaluation be done during IVF treatment?
Uterine evaluation is recommended before IVF or after a failed cycle to rule out hidden uterine factors.
Does treating uterine problems improve IVF success rates?
Yes, identifying and correcting uterine abnormalities can significantly improve implantation and IVF success rates.