Conversations around fertility after 35 have become far more open. Common reasons like career goals, personal choices and improved access to healthcare lead to delayed family planning. At the same time, age and fertility risks are often discussed in ways that can feel alarming or overly simplified, but the reality is completely different.
What Doctors Mean When They Talk about Fertility after 35
Fertility after 35 is usually referred to statistical trends rather than individual outcomes. Research shows a gradual fertility decline after 35, particularly related to egg quality and the time it may take to conceive. This does not mean fertility suddenly stops or that pregnancy after 35 is impossible.
Clinically, age 35 is used as a reference point due to age-related changes and it becomes more noticeable at a population level. For individuals, fertility issues are very personal and influenced by many factors beyond age.
What Actually Changes after 35?
- Egg Quality and Chromosomal Risk
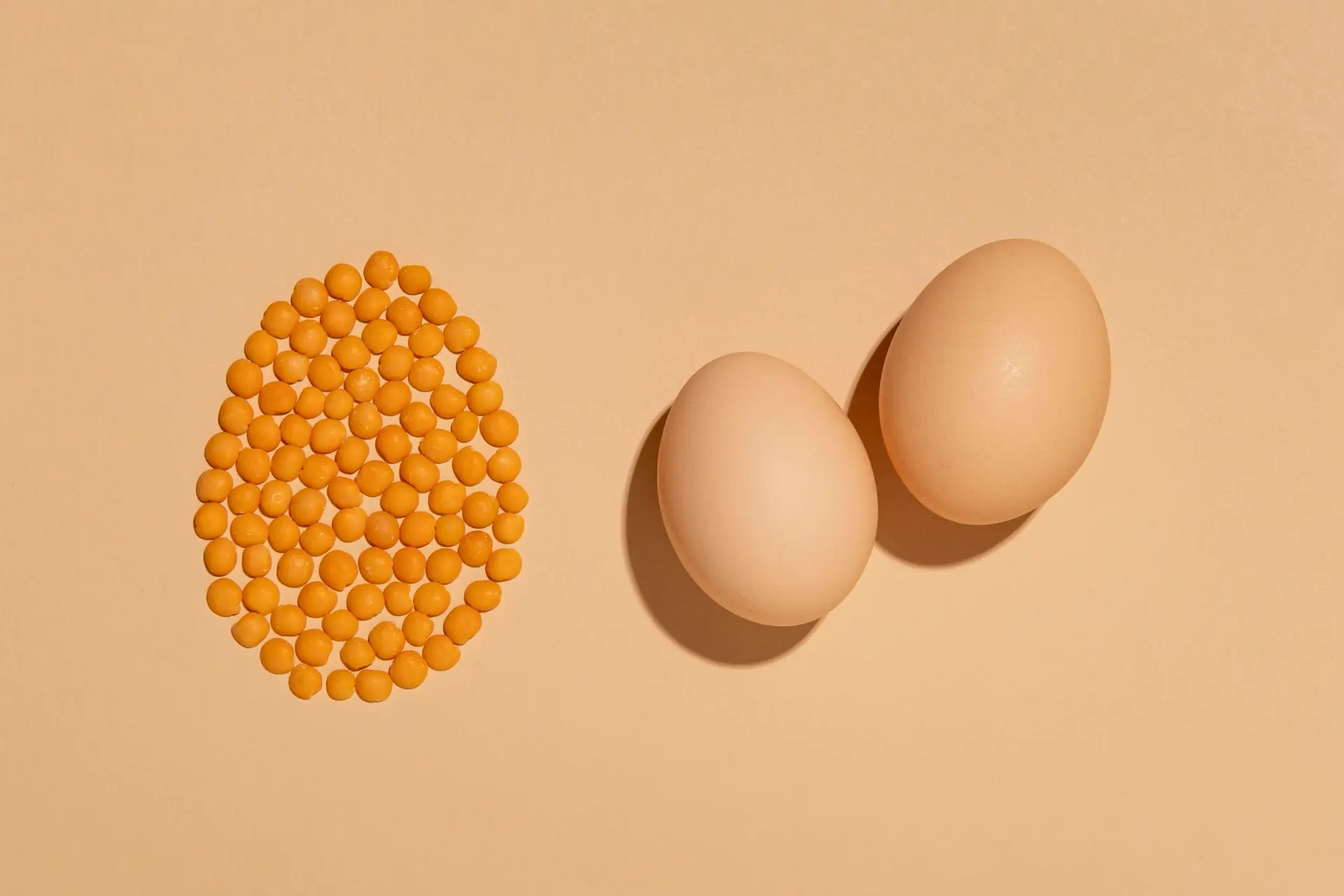
One of the most discussed changes is egg quality after 35. While women are born with all their eggs, the genetic integrity of those eggs changes over time. This increases the chance of chromosomal abnormalities, which can affect implantation or lead to miscarriage. The egg quality also varies widely; age defines probability and not surety for conception.
- Ovulation and Hormonal Shifts After 35
Ovulation patterns can also change slightly with age. If timing is not optimised, hormonal fluctuations lead to shorter cycles or less predictable ovulation, which affect the chances of pregnancy after 35. Study shows that majority of the women in their mid to late thirties continue to ovulate regularly and conceive naturally. These shifts tend to be gradual rather than sudden.
What Doesn’t Change After 35?
Some women continue to ovulate regularly and are able to conceive naturally. Fertility doesn’t stop after 35 in fact, timing matters. Most importantly, fertility varies widely from person to person. Age offers general guidance, but it does not define individual reproductive potential.
Why Age Doesn’t Decide Fertility
One of the biggest misconceptions is that fertility is decided only by age, in reality the ability to conceive does not disappear after 35. Factors such as overall health, menstrual cycles, sperm quality, lifestyle and underlying medical conditions play a significant role. Many conceive without assistance, especially when cycles are regular and other fertility markers are reassuring.
Pregnancy after 35: Risks vs Reality
Pregnancy after 35 is often labelled as high risk, but it can be misleading. Certain conditions like gestational diabetes, chromosomal conditions and blood pressure are statistically higher, most pregnancies after 35 progress without major complications. Latest prenatal care, early screening and close monitoring have significantly improved outcomes. For many, the reality of pregnancy after 35 is far more positive than common narratives suggest.
Age and Fertility Risks
Age and fertility risks are often communicated in percentages that feel abstract. A relative increase in risk does not necessarily correspond to a high absolute risk. For instance, certain complications become more prevalent with advancing age, they still impact a minority of pregnancies overall.
Why Some People Conceive Easily After 35 and Some Don’t
Fertility differs from person to person hence the chances of pregnancy after 35 vary. Ovarian reserve, egg quality, uterine health, sperm factors, and timing all interact in complex ways. Two people of the same age may have very different fertility profiles and this is why assessment matters more than relying on age-based assumptions personalised.
When Fertility Testing Makes Sense After 35
Fertility testing is often recommended earlier for those over 35, especially if pregnancy has not occurred after six months of trying. Testing may include hormone levels, ultrasound assessment of ovarian reserve, and semen analysis. Early evaluation does not mean treatment is inevitable.
Treatment Options after 35: From Natural Support to IVF
Treatment differs from person to person after 35 as some women benefit from tracking cycles, lifestyle changes and addressing hormonal issues, while some consider assisted options such as ovulation induction or IVF, suitable for their fertility profile.
IVF success rates do decline with age, largely due to egg quality, but outcomes vary. Treatment decisions are most effective when guided by individual data rather than age alone.
What Matters More Than Age When Planning Pregnancy
Health is the major factor that plays a vital role in pregnancy, while age is another. Realistic planning and better outcomes can be achieved through a holistic approach that looks beyond numbers.
Trying to Understand Your Fertility after 35?
It is advisable to take fertility specialists opinion for fertility after 35. Right guidance will help you to navigate this phase with clarity and confidence and make decisions that meet your personal and medical objectives.
FAQs
Is it difficult to get pregnant after 35?
It may take longer to conceive, but many people conceive naturally after 35.
What are the real fertility risks after the age of 35?
Risks like changes in egg quality and a higher chance of chromosomal abnormalities, but most pregnancies are healthy.
Is there a possibility of a healthy pregnancy after 35?
Of course, with appropriate care, the majority of pregnancies after 35 progress well.
Does fertility decline suddenly after 35?
Fertility decline after 35 is gradual, not sudden.
When should someone over 35 seek medical advice?
You should consult for medical advice if pregnancy has not occurred after six months of trying, or sooner if there are known concerns.